Medicare obesity drug coverage has become a hot topic as the Centers for Medicare and Medicaid Services (CMS) recently declined to implement a proposal from the Biden Administration that could have expanded coverage for weight-loss drugs such as Wegovy and Zepbound. This decision has significant implications for beneficiaries, as these medications offer vital treatments for obesity, a condition that affects millions of Americans. Currently, while diabetes medications can be reimbursed, anti-obesity versions like Wegovy and Zepbound remain excluded from Medicare coverage under Part D. Advocates for obesity treatment Medicare argue that this limitation not only restricts access but also overlooks the medical understanding of obesity as a chronic disease. The broader implications of this decision may lead to increased healthcare costs due to the health risks that obesity poses, making the need for future policy revisions crucial.
The recent decision regarding the exclusion of weight-loss medications from insurance plans has sparked widespread concern among healthcare advocates. With discussions surrounding obesity treatment under Medicare increasingly prominent, many are questioning the adequacy of available options for managing this prevalent condition. Many individuals suffering from obesity may seek alternative weight management solutions, but without coverage for effective drugs like Wegovy and Zepbound, access remains limited. As these discussions evolve, the focus on how insurance products, particularly Medicare Part D, can better support patients in their weight-loss journeys remains critical. Interest in understanding obesity treatments will likely grow, prompting calls for policy changes that acknowledge the importance of comprehensive coverage.
Understanding Medicare Obesity Drug Coverage
Medicare obesity drug coverage has been a subject of great interest, particularly as the public debate around obesity management continues to grow. The recent decision by the Centers for Medicare and Medicaid Services (CMS) not to cover weight-loss medications like Wegovy and Zepbound has highlighted the challenges within the Medicare system concerning obesity treatment. This decision has wide-reaching consequences, as millions of beneficiaries who struggle with obesity will not have access to these potentially life-saving medications. Many healthcare experts are concerned that this lack of coverage may result in higher long-term healthcare costs.
Obesity medications, while primarily approved for weight loss, have been shown to have numerous health benefits, including reducing risks related to conditions such as heart disease and type 2 diabetes. With the growing body of evidence supporting the therapeutic effects of these drugs, it is increasingly clear that Medicare needs to reevaluate its stance on obesity treatments. Future discussions must consider both the cost-saving potential associated with managing obesity and the importance of recognizing its status as a serious chronic disease.
The Implications of Wegovy Medicare Coverage Denial
The denial of Wegovy Medicare coverage signals a significant setback for many individuals seeking effective treatments for obesity. As it stands, beneficiaries are left with limited options for managing this chronic condition, which affects millions of Americans. The absence of insurance coverage for weight-loss drugs means that many patients might not pursue treatment due to high out-of-pocket costs. This, in turn, can lead to worsening health outcomes as people are unable to afford essential medications that could facilitate weight loss and improve overall health.
Furthermore, the implications extend beyond individual health, affecting healthcare systems and insurance models. As patients choose not to engage with obesity treatments, the long-term consequences could manifest as higher incidences of obesity-related diseases, thus placing a heavier financial burden on the healthcare system. This scenario raises the pressing need for policy changes that align with evolving scientific understanding—acknowledging obesity not merely as a lifestyle choice but as a medical condition that warrants effective management strategies.
Zepbound Insurance Options under Medicare Part D
The absence of coverage for Zepbound under Medicare Part D complicates access to this innovative obesity treatment for millions of beneficiaries. As a medication designed to address obesity, Zepbound has shown promising results in clinical trials, yet its lack of coverage means many eligible individuals may never benefit from its potential. For patients facing high drug costs, the economics of managing obesity become significantly more challenging, and this can ultimately deter them from seeking necessary treatments or adhering to prescribed health plans.
Insurance companies and policymakers must examine the economic ramifications of this gap in coverage. It is essential to advocate for solutions that will allow Zepbound and similar medications to be accessible to all who need them, especially those enrolled in Medicare. The ongoing discussions surrounding insurance policies and obesity treatments indicate a need for a comprehensive approach that includes the cost-effectiveness of coverage, patient access, and long-term health outcomes.
The Future of Obesity Treatment in Medicare
As the nation grapples with rising obesity rates, the future of obesity treatment in Medicare remains uncertain. The current lack of support for weight-loss medications under the program potentially stifles progress in preventive healthcare. Recent statements from pharmaceutical companies like Novo Nordisk and Lilly highlight the urgency with which the issue needs to be addressed. By failing to include drugs like Wegovy and Zepbound, Medicare is not only limiting treatment options but also risking higher healthcare costs in the long run.
The future should entail a critical reevaluation of obesity as a treatable condition that requires support from Medicare and Medicaid. Healthcare experts are advocating for policies that will allow coverage for these drugs, correlating them with better health outcomes and reduced long-term healthcare expenditures. As research continues to unveil the broader benefits of obesity treatments—including potential impacts on health conditions such as kidney disease—it becomes imperative that Medicare policies evolve accordingly.
Key Benefits of Obesity Treatment Drugs
Obesity treatment drugs like Wegovy and Zepbound offer a range of health benefits beyond weight loss. Research suggests that these medications can lower the risk of serious conditions such as cardiovascular diseases and type 2 diabetes, which are prevalent in individuals with obesity. In fact, the FDA has approved these drugs for various health-related benefits, which makes their unavailability under Medicare coverage particularly concerning.
In addition to weight management, obesity drugs help mitigate obesity-related complications, hence providing a strong case for their inclusion in Medicare’s drug benefit plans. By improving beneficiaries’ health outcomes, these medications could ultimately lead to reduced overall healthcare costs associated with chronic diseases, emphasizing the need for policymakers to reconsider coverage limitations.
Navigating Weight-Loss Drugs Coverage with Medicaid
Navigating weight-loss drugs coverage through Medicaid presents its own set of challenges, often varying significantly from state to state. Some states have implemented measures that allow for weight-loss treatments as part of their Medicaid programs, while others have not. This inconsistency can confuse beneficiaries who are trying to understand what treatments are available to them.
As the conversation around obesity treatment continues, Medicaid policymakers must align their coverage policies with the realities of health care needs. Expanding access to medications like Wegovy and Zepbound can create more opportunities for effective obesity management among recipients, addressing the growing health crisis linked to obesity. Ensuring that all Medicaid enrollees have access to necessary treatments is essential for improving public health outcomes related to obesity.
The Role of Congressional Leaders in Obesity Treatment Legislation
Congressional leaders play a critical role in shaping legislation around obesity treatment, influencing how medications like Wegovy and Zepbound are covered by Medicare and Medicaid. The current environment suggests a need for stronger advocacy to ensure obesity is recognized as a treatable condition that requires adequate healthcare support. While pharmaceutical companies express their commitment to working with policymakers, it is essential for legislators to prioritize access to obesity medications as part of a comprehensive healthcare strategy.
From public health perspectives, enabling access to effective weight-loss treatments can directly affect productivity and overall well-being of the population. As discussion surrounding obesity treatment legislation heats up, it remains imperative for members of Congress to advocate for policies that support drug coverage, ensuring that no individual living with obesity is left without treatment options.
Examining the Cost-Effectiveness of Weight-Loss Drugs
The cost-effectiveness of weight-loss drugs is an essential aspect of the ongoing debate about their coverage under Medicare and Medicaid. Although the upfront costs of medications like Wegovy and Zepbound can seem prohibitive, analysis indicates that their use can result in significant savings by preventing the onset of obesity-related illnesses. Therefore, failing to cover these medications could ultimately lead to higher long-term healthcare expenses due to increased morbidities associated with untreated obesity.
Financial considerations are crucial for policymakers when evaluating the benefits of weight-loss drug coverage. By understanding the broader economic impacts of investing in obesity treatments, including potential savings in disease management and improved quality of life, stakeholders can build a compelling case for enhanced coverage options. As the healthcare landscape evolves, incorporating these insights into legislative frameworks will be vital.
The Impact of New CMS Initiatives on Obesity Management
The new initiatives being proposed by CMS regarding obesity management represent a pivotal moment in the insurance landscape, particularly for Medicare. As the organization reviews and adjusts its policies, the potential inclusion of weight-loss drugs under Medicare coverage would significantly alter the treatment landscape. These changes could facilitate better access to medications that aid in effective weight management, ultimately addressing the needs of millions of beneficiaries.
Engaging with stakeholders, including healthcare professionals and patients, will be vital as CMS navigates these new initiatives. By promoting evidence-based recommendations and maintaining open channels for feedback, CMS can work towards creating a framework that effectively incorporates obesity treatment drugs into the Medicare system. This evolution reflects the growing recognition of obesity as a serious health concern that necessitates comprehensive management strategies.
Frequently Asked Questions
What is Medicare obesity drug coverage and which medications does it include?
Medicare obesity drug coverage refers to the potential for Medicare beneficiaries to receive reimbursement for medications that treat obesity. Currently, weight-loss drugs such as Wegovy and Zepbound are not covered under Medicare, despite being effective treatments for obesity. While Medicare covers diabetes medications, the anti-obesity versions will not be reimbursed as of now.
Is Wegovy covered by Medicare for obesity treatment?
As of the latest announcement, Wegovy is not covered by Medicare for obesity treatment. Although it is an effective drug for weight loss, the Centers for Medicare and Medicaid Services (CMS) has decided not to move forward with its coverage under Medicare Part D.
What can beneficiaries do about the lack of Medicare obesity treatment coverage?
Beneficiaries affected by the lack of Medicare obesity treatment coverage can explore options through private insurance plans, or Medicare Advantage plans that may offer coverage for weight-loss drugs. It’s also advisable to speak with healthcare providers about alternative treatments or to advocate for policy changes regarding Medicare obesity drug coverage.
What is Zepbound and does Medicare cover it for weight loss?
Zepbound, developed by Lilly, is specifically designed for obesity treatment, similar to Wegovy. Unfortunately, as of now, Medicare does not provide coverage for Zepbound as an obesity treatment, reflecting the current stance on Medicare obesity drug coverage.
Why has Medicare not expanded coverage for weight-loss drugs like Wegovy and Zepbound?
Medicare has opted not to expand coverage for weight-loss drugs like Wegovy and Zepbound due to concerns about increasing government spending and limited evidence on the long-term effects of these medications. This decision affects many beneficiaries who could benefit from obesity treatment.
Are there any recent changes regarding Medicare Part D and obesity treatment coverage?
Recent announcements indicate that there have been no changes to Medicare Part D regarding obesity treatment coverage. The Biden Administration’s proposal to include weight-loss drugs like Wegovy and Zepbound under this program has not advanced, leaving current policies unchanged.
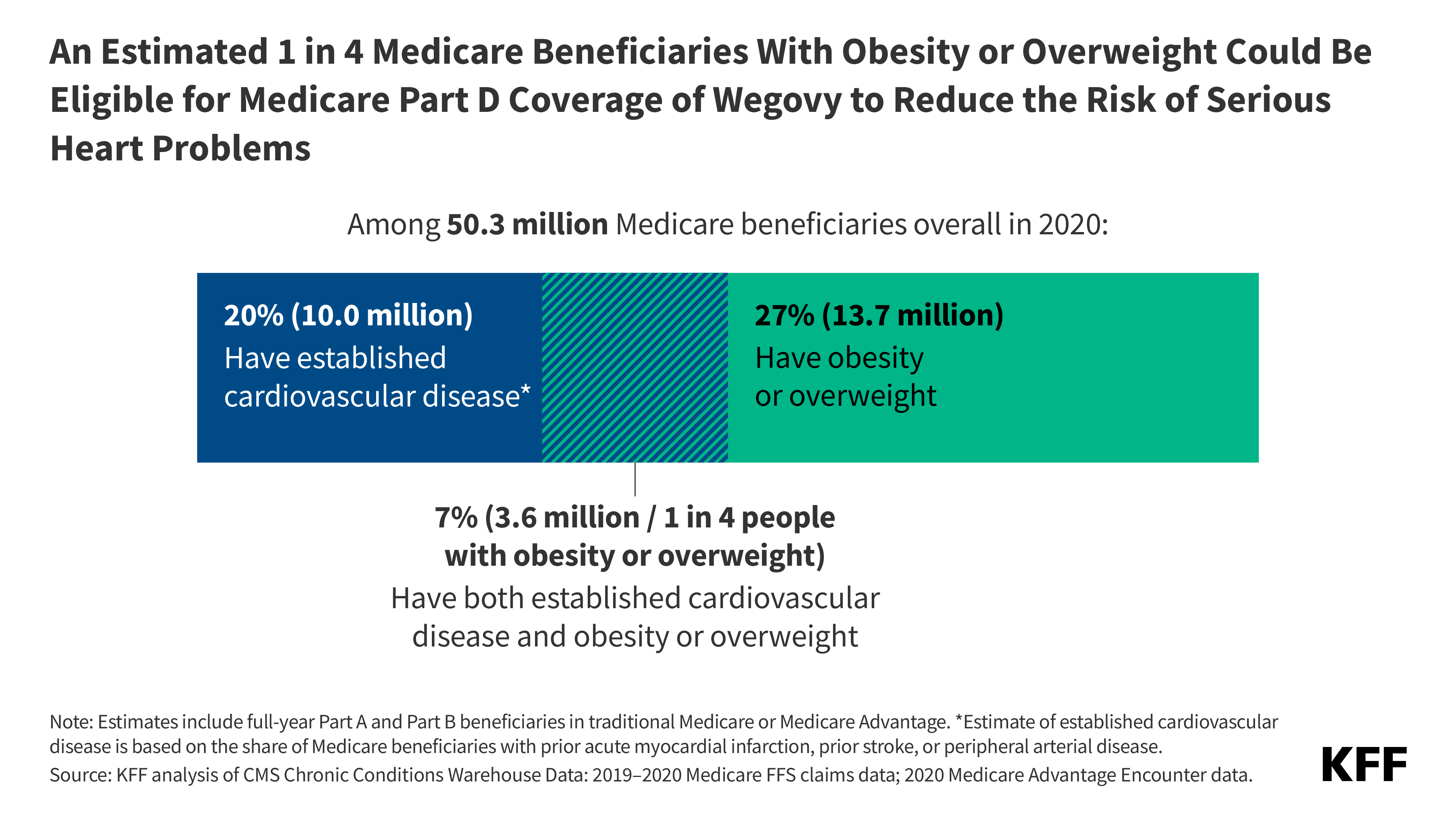
How many Medicare recipients are affected by the lack of obesity drug coverage?
Approximately 7.5 million Medicare and Medicaid recipients are impacted by the lack of coverage for weight-loss drugs like Wegovy and Zepbound, as they will not receive reimbursement for these medications under existing Medicare policies.
What is the potential impact of denying Medicare obesity treatment coverage on healthcare costs?
Health experts suggest that denying coverage for effective obesity treatments could lead to higher long-term healthcare costs for insurers. This is because these drugs may offer additional health benefits, such as reduced risks for heart disease and other chronic conditions, which could ultimately save money in the healthcare system.
Will future decisions change Medicare coverage for obesity drugs?
While current decisions on Medicare coverage for obesity drugs remain unchanged, there is hope that with the confirmation of new leadership at CMS and ongoing discussions with health advocates, coverage policies may eventually evolve to reflect scientific advancements and recognize obesity as a chronic disease needing treatment.
| Key Point | Details |
|---|---|
| Medicare’s Decision | CMS announced it will not implement a proposal to cover weight-loss drugs for beneficiaries. |
| Drugs Affected | Wegovy and Zepbound, which are both used for obesity treatment, remain uncovered. |
| Comparison with Diabetes Drugs | Wegovy has a higher dosage for obesity, while Zepbound aligns with a diabetes medication, Mounjaro. |
| Impact on Beneficiaries | Nearly 7.5 million Medicare and Medicaid recipients will not receive drug reimbursements. |
| Statements from Manufacturers | Spokespersons from Novo Nordisk and Lilly expressed disappointment with the decision, emphasizing the need for obesity coverage. |
| Long-Term Effects and Concerns | Health experts warn of possible increased costs due to denying coverage, despite potential health benefits of these drugs. |
Summary
Medicare obesity drug coverage has faced a significant setback following the recent announcement by the Centers for Medicare and Medicaid Services (CMS) not to include weight-loss medications, such as Wegovy and Zepbound, in its coverage plans. This decision affects millions of beneficiaries who could benefit from these drugs aimed at treating obesity, a condition now recognized as a serious chronic disease. Stakeholders argue that this lack of coverage may lead to greater long-term health costs due to untreated obesity-related conditions, contradicting the intended savings from not reimbursing these medications.